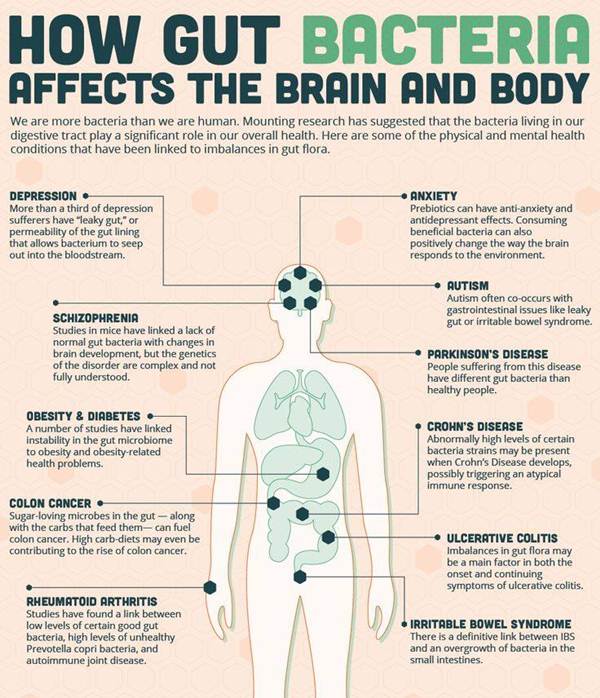
There has been a growing understanding and exploration by psychologists, psychiatrists, physicians and researchers about the role our gut bacteria plays on our mood—most notably the experience of anxiety.
The statistics on anxiety are staggering and trending north each passing year. Consider these stats: According to the Anxiety and Depression Association of America (and NIMH) anxiety is the most common mental illness in America today.
An estimated 40 million adults (18 and older) or 18 percent of the population endorse symptoms of anxiety (not to mention one out of eight children). Treatment of anxiety accounts for one-third of the $148 billion dollars spent annually on mental illnesses in America.
The symbiotic relationship between our gut health and how we feel is a hot topic of discussion and research. Scientists, physicians, and mental health practitioners are increasingly aware of the important relationship between the balance of “critters” in our gut and how we experience our brain, mood and emotions. So, before we begin to discuss what we can do to optimize this important relationship, let’s explore the underlying processes.
From a holistic vantage point our gut is known as the “second brain” and there are structural/anatomical reasons for this reference. The “second brain,” known scientifically as the enteric nervous system, consists of sheaths of neurons located in the walls of our gut. We refer to these sheaths as the vagus nerve and it runs from our esophagus to our anus, roughly nine meters long.
The bacteria, fungi and viruses that make up your body’s microflora outnumber your body’s cells by 10 to 1.
95 percent of the body’s serotonin supply is found in our bowels.
The vagus nerve contains 100 million neurons, which is more neurons than the spinal cord or peripheral nervous system hold.
There are over 100 trillion bacterial cells contained within the gut.
Our gut sends far more information to our brain than the other way around.
When the precarious balance of bacteria in our gut becomes disturbed we often experience symptoms associated with Irritable Bowel Syndrome and other gastrointestinal related disorders. These symptoms are likely to start out as complaints of bloating, gas, constipation or diarrhea.
These symptoms are often indicators of “leaky gut syndrome” where our gut wall becomes permeable and particles of food start to escape from the digestive and GI tract. When this occurs the domino effect of issues becomes inevitable and thus begins the cascading symptom patterns that plague tens of millions of Americans struggling with GI related disorders.
Due to the interconnectedness of our brain and enteric nervous system, via the vagus nerve, once our gut bacteria is out of whack, we are vulnerable to a pattern of emotional discomfort, usually marked by increasing episodes of anxiety and depression.
How does our gut bacteria become so unbalanced? Here are a few of the many ways in which we accidentally (and sometimes unavoidably) contribute to this pattern of disturbance:
Excessive and unmanaged stress
Too much use of antibiotics
Prolonged use of steroids
Intestinal infections
High sugar; low fiber diet (in other words, standard American diet)
Regular consumption of alcohol
If you are reading this blog and you find yourself relating to this content, I encourage you to seek out professional help to better understand what these symptoms mean for your unique constitution. Taking the right type of probiotic to help restore balance in the micro flora in your gut is one step, but often with more advanced GI issues and more acute anxiety based symptoms there is a need to first heal the permeability of the gut wall before adding in probiotics.
There is a growing body of research that is exploring strain specific probiotics to help mitigate acute symptoms of anxiety. For example, in clinical trials involving the study of mice, Bifidobacterium longum and Lactobacillus Rhamnosus have shown to help normalize anxiety-like behavior. Lactobacillus appears to work on the GABA receptors, an inhibitory neurotransmitter involved in the regulation of acute anxiety. GABA is the receptor influenced when you take a benzodiazepine such as Xanax or Ativan.
There is a bourgeoning area of interest and research exploring use of probiotics to treat a wide variety of mental illnesses. Pharmaceutical companies are attempting to create a new line of psychiatric medications referred to as Psychobiotics, but this field of research is still in its infancy.
So, that being said, there is a lot we can do right from the comfort of our own home to start the process of realigning the balance of our gut flora. As you can imagine, most of it involves cleaning up our diet, being mindful of the relationship between food and mood, and exploring our habits and patterns. Below are action steps you can take in an effort to begin the process of healing your gut, mind and brain:
It generally takes a minimum of 90 days for these suggestions to be maximally effective:
- Eliminate sugars: The “fake” sugars. We are not talking about eliminating whole fruits. Rather, cutting out the baked goods, cookies, ice cream, and store bought sugary products that wreak havoc on the bacteria in our gut and lead to cyclical patterns of emotional and physical cravings.
- Eliminate all simple starches and reduce intake of even complex starches.
- Add in fermented and living foods. Please try to avoid store bought yogurts even though they are considered fermented. These products are loaded with sugars and often end up exacerbating imbalance.
- Consider having the vast majority of your diet be plant-based foods. Generally speaking, eat as many veggies as you want in any form you want. Avoid use of store bought dressings etc., which are loaded with sugar and preservatives. If your GI tract is especially damaged, consider cooking all your veggies before consumption.
- Consume foods high in Omega-3 fatty acids (walnuts, salmon, flax, some types of squash, etc.).
- Aim to consume local and organic sources of animal protein. Doing so will reduce your ingesting unwanted antibiotics and feed based chemicals.
- Discuss with your practitioner if the use of a probiotic or prebiotic will benefit your unique situation. A probiotic introduces specific strains of good bacteria, while a prebiotic introduces carbohydrates that serve as food the bacteria already present in your gut.
- Exercise. Again, more days than not. Enough to sweat. The goal is to find joy in it. But if you hate it, that’s okay. Do it anyway.
- Drink mostly water.
- Work with a skilled psychologist or mental health professional to metabolize past trauma, identify faulty thought patterns, and implement mindfulness based skills to better manage your central nervous system.
- Implement a daily mindfulness/meditation practice. The goal is observe your mind, not to clear it or control your thoughts. Simple observation and balanced breathing. This is a restful and restorative way to calm the central nervous system and recalibrate the vagus nerve.
Exploring the relationship between our mood and our gut bacteria reveals an interconnected relationship between the mind, brain, and body, via the enteric nervous system and vagus nerve. This relationship is the foundation of why it is critical to address your emotional discomfort from a holistic and integrated approach to your wellness.
The good news is that because we now know and understand that there is a connection between the mind and body, we have the knowledge and tools to make immediate changes that will yield significant results in how we feel. The better we understand and participate in our own sense of wellness and empowerment the more likely we are to embark on change that starts from within.
By Dr. Sarah Sarkis for elephant journal
 Sarah Sarkis is a licensed psychologist living in Honolulu, Hawaii. She has a private practice working with adults in long-term insight-oriented therapy. She works with an existential psychology vantage point, encouraging patients to “stay present even in the storm.” She is an explorer of the psyche, emphasizing collaboration, partnership, and personal empowerment. She approaches psychological wellness from a holistic and integrative perspective. Her therapeutic style is based on an integrative approach to wellness, blending strong psychodynamic and insight-oriented training with more traditionally behavioral and/or mind/body techniques to help clients foster insight, change and growth. She has extensively studied the connection between mindfulness, functional medicine, hormones, and food, medicine and mood. Find out more at her blog.
Sarah Sarkis is a licensed psychologist living in Honolulu, Hawaii. She has a private practice working with adults in long-term insight-oriented therapy. She works with an existential psychology vantage point, encouraging patients to “stay present even in the storm.” She is an explorer of the psyche, emphasizing collaboration, partnership, and personal empowerment. She approaches psychological wellness from a holistic and integrative perspective. Her therapeutic style is based on an integrative approach to wellness, blending strong psychodynamic and insight-oriented training with more traditionally behavioral and/or mind/body techniques to help clients foster insight, change and growth. She has extensively studied the connection between mindfulness, functional medicine, hormones, and food, medicine and mood. Find out more at her blog.




















Sorry, the comment form is closed at this time.